Gene Therapy in Sickle Cell
Sickle Cell
Sickle cell anemia is associated with low calcium intake, vitamin D deficiency, and nutrient deficiency. Staying hydrated and eating a good diet is important as ever for staying healthy with sickle cell. Working with a nutritionist can help you develop a plan that works for your body.
Hemoglobin
cells of the immune system that help defend the body against infection
Reticulocytes
immature red blood cells that form and mature in the bone marrow before being released into the blood
Platelets
tiny blood cells that help the body form clots to stop bleeding
White blood cells
cells of the immune system that help defend the body against infection
Learn more about the genetic cause of sickle cell and available treatment options, including gene therapies that work by using your own cells.
Learn more about the genetic cause of sickle cell and available treatment options, including gene therapies that work by using your own cells.
Understanding how to address sickle cell at the genetic level Understanding how to address sickle cell at the genetic level
Understanding how to address sickle cell at the genetic level Understanding how to address sickle cell at the genetic level
For nearly 100 years, scientists have studied the human body and the building blocks of DNA. With each mark of progress comes a better understanding of how our bodies work at the DNA or genetic level.
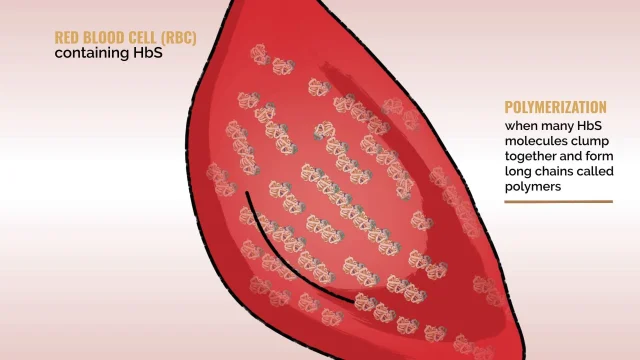
Sickle cell disease is a lifelong, genetic illness caused by a mutation in a gene at the DNA level. The mutation affects the normal adult hemoglobin (HbA) gene, leading the body to produce an abnormal form of hemoglobin called sickle hemoglobin (HbS). This can cause red blood cells to form in the shape of a sickle. Gene therapy may be one way to help address this problem.
Two examples of gene therapy in sickle cell include gene addition and gene editing. In both types, your own cells are collected, modified, and reintroduced to your body with the objective of providing new instructions to create hemoglobin.
Gene Addition
Gene addition therapy is the process of adding modified working copies of a gene to stem cells, collected from a person, to provide a new set of instructions for cells.
So, for individuals with sickle cell disease, that would be adding a working gene that instructs the body to produce a functioning form of hemoglobin that can compensate for sickle hemoglobin.
A vector helps deliver the gene to your cells
The delivery system responsible for delivering the working copies of a modified hemoglobin gene to your cells is called a vector. There are viral vectors (those based on a virus) and non-viral vectors. One of the most widely used and studied viral vector types is a lentiviral vector. The most well-studied lentivirus is human immunodeficiency virus (HIV), and scientists have used its blueprint to design lentiviral vectors for gene therapy. The reason scientists create vectors based on viruses is because viruses are very efficient at delivering genetic material to cells of the body. Though vectors are based on viruses, they do not contain any of the parts of the virus that can cause an infection. Vectors act as a delivery system into cells.


Gene Editing
Like gene addition, gene editing requires the collection of stem cells to start the process.
Gene editing modifies a person’s DNA by either changing a mutated gene directly or by changing a related gene to compensate for the mutated one. Changing a related gene means turning the on/off switch for a different gene that regulates the production of a type of hemoglobin produced by your body. This switch helps the body increase production of a working type of hemoglobin protein.
One example of gene editing technology is known as CRISPR-Cas9 (Clustered Regularly Interspaced Short Palindromic Repeats), which is found in bacteria. CRISPR uses a delivery system called electroporation. This nonviral technology uses electricity to enable DNA to pass through cell membranes.


In addition to gene editing and gene addition, there are other types of gene therapy being studied as part of the greater sickle cell disease treatment landscape, like gene correction and gene silencing. These different types of gene therapy continue to evolve rapidly, with many current and upcoming clinical trials underway to investigate their potential as treatment options for sickle cell disease.
Gene Therapy Treatment Process
The treatment process for gene therapy relies on close collaboration between a patient and their primary physician, their treatment team, and their caregivers. It's important to keep in mind that there are a lot of things to consider when learning about gene therapy. It can be a detailed process—one that takes place over a long period of time, often with many consultations and visits. That’s why staying informed and having as many conversations as needed are important aspects of the process.
In general, there are 4 steps to the treatment process: consultation, preparation, treatment, and recovery. Let’s take a quick glance at each step:
STEP 1: CONSULTATION

STEP 1: CONSULTATION
- Discuss the potential risks and benefits of the specific gene therapy
- Ensure appropriateness and eligibility of gene therapy. This can include discussions around your or your loved one’s physical and emotional health, as well as the existing support network
- If you or your loved one decides to discuss or move forward with gene therapy, you or your loved one will need to go through a process called informed consent. Informed consent is where a patient actively participates in discussions with their physician and is empowered to make decisions about their medical care by deciding which treatments they do (or do not) want
- Discuss any short- and long-term steps to plan for gene therapy, including healthcare coverage, fertility discussions, timing of treatment, chemotherapy, side effects of gene therapy, and any potential impacts on life, family, and work
- This consultation step can take weeks or months, depending on discussions between you or your loved one and the treating physician/treatment team and the timing of the referral. These discussions can include multiple consultations with specialists or physicians at a specialized treatment center with an expertise on gene therapy
- You or your loved one's primary physician and care team at the treatment center will work with you to collectively determine if gene therapy is the appropriate treatment choice
STEP 2: PREPARATION

STEP 2: PREPARATION
- Will include the stem cell collection needed for manufacturing gene therapy ex vivo (meaning created outside your body)
- Physician will give instructions for any preparation procedures or regimens that you or your loved one will need to complete
- Usually requires a few days for the patient to stay in the hospital for stem cell collection. After the collection, it will usually take a few months for the lab to modify the patient’s own stem cells to create the gene therapy
STEP 3: CONDITIONING WITH CHEMOTHERAPY

STEP 3: CONDITIONING WITH CHEMOTHERAPY
- Conditioning with chemotherapy happens at this stage—conditioning is needed for all transplant-based treatments to help maximize the effects of treatment by clearing out the cells that contain the mutated hemoglobin gene and making room in the bone marrow for the modified stem cells
- Treatment with chemotherapy includes certain risks, including fertility, which you should discuss with your doctor
STEP 4: TREATMENT

STEP 4: TREATMENT
- Gene therapy treatment that was prepared using your (if you’re a caregiver, your loved one’s) own cells is infused back in. Treatment is often administered by a specialist and can include a specialized care team
- After treatment, you or your loved one will remain in the hospital for several weeks—this time span includes a recovery period and the time needed for engraftment and monitoring. Engraftment is when transplanted stem cells enter the blood and make their way to the bone marrow to start making new blood cells
STEP 5: RECOVERY/LONG-TERM FOLLOW-UP

STEP 5: RECOVERY/LONG-TERM FOLLOW-UP
- You will be discharged once your physician has decided it is safe for you or your loved one to leave the hospital
- May include follow-up appointments at the specialized treatment center and with you or your loved one’s physician
- May include home healthcare for a period of time
- May include enrolling in a registry to monitor long-term treatment results
- After gene therapy is administered, there is a critical process of recovery and a follow-up monitoring period that can last for at least 15 years. If you or your loved one is treated with gene therapy, you will work with your physician to monitor the effect of treatment during this period. You or your loved one may be asked whether you’re interested in enrolling in registries to help track the long-term outcomes of treatment
There Are Some Risks Associated With the Gene Therapy Process
Like any treatment, there are risks associated with gene therapy. Some risks of gene therapy include, but are not limited to:
- Conditioning: Conditioning with chemotherapy can cause a number of side effects. Some side effects can happen quickly including hair loss, rash, nausea or vomiting, and infections, some of which can be life-threatening. Other side effects that can take longer to show up are tooth and mouth issues, not being able to have children, cancers, or liver or bone damage
- Platelet engraftment failure: Platelets are the blood cells that help blood to clot. An engraftment failure could prevent new platelets from developing, which causes the risk for bleeding
- Neutrophil engraftment failure: Neutrophils are the most common type of white blood cell in your immune system, which is the reason an engraftment failure makes you more susceptible to infection
And There are Some Risks Associated With Gene Therapy
- Hematologic malignancy: This can develop from abnormal blood cells produced in the bone marrow. Stress on the body from stem cell collection and chemotherapy may increase the risk of hematologic malignancy. In addition, people with sickle cell disease have an increased risk of developing hematologic malignancies
- Insertional Oncogenesis: In gene addition, the new genes from the vector insert into the DNA of the person’s stem cell via a process called integration. With this process comes a chance that the integration of the new DNA may change the activity of nearby genes, which could cause changes like uncontrolled cell growth, resulting in blood cancer. Individuals receiving gene therapy should be monitored lifelong by their physician for the development of blood cancer
- Off-Targeting: In gene editing, there is a chance that the technique used could make changes at a different site than intended, posing the risk of causing changes to healthy genes
- Unintentional Gene Inactivation: In any type of gene therapy, there comes a risk of unexpected complications that could prevent the function of another important gene, possibly leading to tumor formation and cancer
Spark the Conversation
Discussing your thoughts, questions, and any specific concerns with your doctor is the best way to learn more about gene therapy. Don’t be afraid to ask your doctors questions about sickle cell disease, including current treatment options and treatments that are still being investigated.
Learn more about gene therapy by exploring some of these resources:
- American Society of Gene and Cell Therapy: provides information for patients and their families on science, technology, and gene and cell therapy
- National Human Genome Research Institute: an organization that collaborates with the scientific and medical communities to provide the latest information about the human genome
- oneSCDvoice: a sickle cell–specific platform aiming to connect the sickle cell community and provide educational resources, including a gene therapy education center
bluebird bio, Inc. is not responsible for the content provided by third-party sites or organizations, nor does bluebird bio, Inc. endorse the content of these sites or organizations. This is not a comprehensive list of resources, and it is provided for reference only.